Glaucoma frequently asked questions.
- What is Glaucoma?
- How common is Glaucoma?
- Is Glaucoma inherited?
- Types of Glaucoma
- Can Glaucoma be treated?
- How can Glaucoma be detected?
- Treatment of Glaucoma
What is Glaucoma?
Glaucoma is an eye disease where the optic nerve located at the back of the eye becomes damaged. In approximately half of cases a high pressure inside the eye (intraocular pressure) is the cause, however in some cases there is a normal intraocular pressure and other factors are involved.
The loss of vision in glaucoma is permanent, but with early treatment, the damage to vision can be minimised.
Most patients with glaucoma are not aware of problems with their vision. This is because the central vision (for reading and recognising people) is only affected when glaucoma has advanced to a late stage. Even when central vision is still good, glaucoma may affect the vision needed for driving and getting about (for instance, seeing steps). Blindness from glaucoma is rare. If blindness does occur, it is usually because the glaucoma is already advanced when it is first diagnosed, because the eye pressure has not responded well to treatment or because patients have not taken their drops regularly. For most glaucoma sufferers, the main effect of the condition is the inconvenience of taking eye drops, although laser treatments and Minimally Invasive Glaucoma Surgery (MIGS) are now available that offer alternatives to eyedrops in some cases.
How common is Glaucoma?
Glaucoma of some type is found in about 2 per cent of the population over the age of 40. It can also affect children and young adults, although much less frequently. It is estimated that more than 500,000 people suffer from glaucoma in England and Wales alone, with more than 70 million people affected across the world. The great majority of those with glaucoma have a chronic (slowly developing) form of the condition, primary open angle glaucoma (POAG), and studies have demonstrated that half of all cases remain undiagnosed.
Is Glaucoma inherited?
Close blood relatives of patients with POAG have at least a four-fold increased risk of glaucoma compared with those without a family history of glaucoma. People from families in which a member has glaucoma should be tested for glaucoma from the age of 35 onwards. People with other glaucoma risk factors in addition to the family history (e.g. being of African-Caribbean origin or having diabetes) should be tested from an even earlier age.
Types of glaucoma
There are 2 main types of glaucoma:
Open-angle – where the angle between the peripheral cornea and iris is open
Closed-angle – where this angle is closed
The angle is the approach to the ‘plughole’ for fluid to exit the eye. If this angle is closed then fluid cannot readily exit the eye and the pressure in the eye rises leading to damage to the optic nerve (glaucoma). In open angle glaucoma the plughole itself is affected (‘silted up’) and this leads to a rise in intraocular pressure.
Can Glaucoma be treated?
The treatment of glaucoma has developed considerably over recent years and new, more potent drugs with fewer side effects than earlier medications are now available. Surgical techniques have also improved and it is estimated that around 95 per cent of those diagnosed early with glaucoma in the UK will retain useful sight for life.
How can glaucoma be detected?
The most common form of glaucoma (Primary Open Angle Glaucoma (POAG) is sometimes not detected by patients until it has got to an advanced stage. This can be because:
- An unaffected eye can ‘fill in’ for the other.
- The detailed central vision is not affected until a late stage.
- People wrongly assume that the reduction in their vision is simply due to age.
Everyone over 40 years of age should ensure that they have regular sight tests every two years to discover if their eyesight has deteriorated. These tests are a good opportunity to check for any signs of glaucoma.
During these visits, make sure you ask the optometrist (optician) to carry out the three glaucoma tests.
The three glaucoma tests are:
- Eye Pressure (Tonometry):- Tonometry is the measurement of intraocular pressure (the pressure inside the eye) and can be carried out with several different instruments.
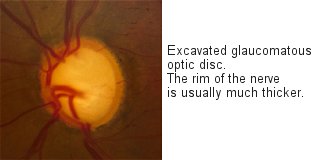
- Optic Disc Appearance (Ophthalmoscopy):- The appearance of the optic disc can be examined using an ophthalmoscope(a special sort of torch) or by the use of a slit lamp. This allows the examiner to assess the degree of cupping of the optic disc and the health of the retina.
- Visual Field (Perimetry):- Perimetry is the technique of mapping out the blank or less sensitive areas in the field of vision, so that the presence of optic nerve damage can be assessed. An online version of a visual field test can be found at www.testvision.org
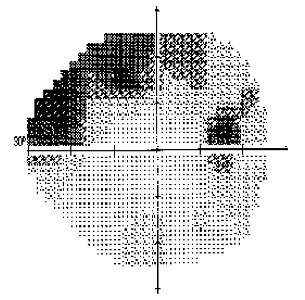
A visual field of an eye with glaucoma. The darker areas are areas where the instrument has detected loss of function of some areas of the retina caused by glaucoma. The peripheral areas are usually affected first.
These three tests together increase the likelihood of glaucoma detection by four times when compared with Ophthalmoscopy alone.
The three tests are quick and painless and, depending on the instruments used, should only take around 15 minutes in addition to the normal eye examination.
Treatment of Glaucoma
The loss of vision in glaucoma is permanent, but with early treatment, the damage to vision can be minimised. In some patients, the loss of vision occurs very slowly and treatment may not be necessary. However, most patients do require treatment. This prevents or slows further loss of vision in most patients. Taking the treatment is important, even though the vision may seem normal, because the loss of vision may get worse without the patient noticing.
All treatment for glaucoma is designed to reduce the level of intraocular pressure to a point at which further damage to the optic nerve is prevented. This reduction in the level of intraocular pressure is achieved by a variety of means including eye drops, tablets, laser treatments for glaucoma and surgery for glaucoma. Each has advantages and disadvantages and the choice of the glaucoma management regime best suited to an individual patient should be made as a collaborative decision involving the patient and the ophthalmologist.
Eye drops usually form the first stage of treatment for glaucoma. There are now a wide variety of eye drops which work in a number of different ways. Most commonly the drops act to reduce the amount of aqueous humour being produced by the ciliary body, some increase the outflow of aqueous humour from the eye either by the conventional outflow pathway through the trabecular meshwork, or by the non-conventional outflow pathway (also known as the uveoscleral outflow pathway), and some do some of each.
The only tablet commonly used in the treatment of glaucoma is Diamox, which is a very powerful type of water tablet. It is most commonly used in the short term treatment of acute angle closure glaucoma prior to laser iridotomy and is rarely prescribed for long term use due to its side effect profile.
Lasers are used to treat both open and closed angle glaucomas with different lasers and different techniques used according to need.
There are also a variety of types of surgery for glaucoma depending on the individual needs of the patient.
Treatment for glaucoma is effective and in the vast majority of cases useful sight can be retained for life providing the treatments are used properly and the agreed management regime followed.